Evidence over hysteria — COVID-19
It is important to note that in both scenarios, the total number of COVID-19 cases will be similar. “Flattening the curve”’s focus is a shock to the healthcare system which can increase fatalities due to capacity constraints. In the long-term, it isn’t infection prevention. Unfortunately, “flattening the curve” doesn’t include other downsides and costs of execution.
Both the CDC and WHO are optimizing virality and healthcare utilization, while ignoring the economic shock to our system. Both organizations assume you are going to get infected, eventually, and it won’t be that bad.
A low probability of catching COVID-19
The World Health Organization (“WHO”) released a study on how China responded to COVID-19. Currently, this study is one of the most exhaustive pieces published on how the virus spreads.
The results of their research show that COVID-19 doesn’t spread as easily as we first thought or the media had us believe (remember people abandoned their dogs out of fear of getting infected). According to their report if you come in contact with someone who tests positive for COVID-19 you have a 1–5% chance of catching it as well. The variability is large because the infection is based on the type of contact and how long.
The majority of viral infections come from prolonged exposures in confined spaces with other infected individuals. Person-to-person and surface contact is by far the most common cause. From the WHO report, “When a cluster of several infected people occurred in China, it was most often (78–85%) caused by an infection within the family by droplets and other carriers of infection in close contact with an infected person.
From the CDC’s study on transmission in China and Princess Cruise outbreak -
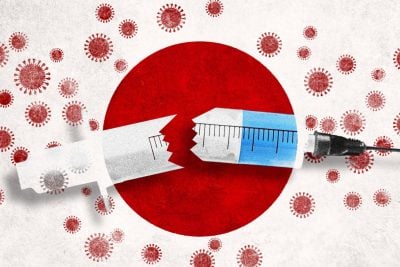
A growing body of evidence indicates that COVID-19 transmission is facilitated in confined settings; for example, a large cluster (634 confirmed cases) of COVID-19 secondary infections occurred aboard a cruise ship in Japan, representing about one fifth of the persons aboard who were tested for the virus. This finding indicates the high transmissibility of COVID-19 in enclosed spaces
Dr. Paul Auwaerter, the Clinical Director for the Division of Infectious Diseases at Johns Hopkins University School of Medicine echoes this finding,
“If you have a COVID-19 patient in your household, your risk of developing the infection is about 10%….If you were casually exposed to the virus in the workplace (e.g., you were not locked up in conference room for six hours with someone who was infected [like a hospital]), your chance of infection is about 0.5%”
According to Dr. Auwaerter, these transmission rates are very similar to the seasonal flu.
Air-based transmission or untraceable community spread is very unlikely. According to WHO’s COVID-19 lead Maria Van Kerkhove, true community based spreading is very rare. The data from China shows that community-based spread was only a very small handful of cases. “This virus is not circulating in the community, even in the highest incidence areas across China,” Van Kerkhove said.
“Transmission by fine aerosols in the air over long distances is not one of the main causes of spread. Most of the 2,055 infected hospital workers were either infected at home or in the early phase of the outbreak in Wuhan when hospital safeguards were not raised yet,” she said.
True community spread involves transmission where people get infected in public spaces and there is no way to trace back the source of infection. WHO believes that is not what the Chinese data shows. If community spread was super common, it wouldn’t be possible to reduce the new cases through “social distancing”.
“We have never seen before a respiratory pathogen that’s capable of community transmission but at the same time which can also be contained with the right measures. If this was an influenza epidemic, we would have expected to see widespread community transmission across the globe by now and efforts to slow it down or contain it would not be feasible,” said Tedros Adhanom, Director-General of WHO.
An author of a working paper from the Department of Ecology and Evolutionary Biology at Princeton University said, “The current scientific consensus is that most transmission via respiratory secretions happens in the form of large respiratory droplets … rather than small aerosols. Droplets, fortunately, are heavy enough that they don’t travel very far and instead fall from the air after traveling only a few feet.”
The media was put into a frenzy when the above authors released their study on COVID-19’s ability to survive in the air. The study did find the virus could survive in the air for a couple of hours; however, this study was designed as academic exercise rather than a real-world test. This study put COVID-19 into a spray bottle to “mist” it into the air. I don’t know anyone who coughs in mist form and it is unclear if the viral load was large enough to infect another individual As one doctor, who wants to remain anonymous, told me, “Corona doesn’t have wings”.
To summarize, China, Singapore, and South Korea’s containment efforts worked because community-based and airborne transmission aren’t common. The most common form of transmission is person-to-person or surface-based.
Common transmission surfaces
COVID-19’s ability to live for a long period of time is limited on most surfaces and it is quite easy to kill with typical household cleaners, just like the normal flu.
COVID-19 be detected on copper after 4 hours and 24 hours on cardboard.
COVID-19 survived best on plastic and stainless steel, remaining viable for up to 72 hours
COVID-19 is very vulnerable to UV light and heat.
Presence doesn’t mean infectious. The viral concentration falls significantly over time. The virus showed a half-life of about 0.8 hours on copper, 3.46 hours on cardboard, 5.6 hours on steel and 6.8 hours on plastic.
According to Dylan Morris, one of the authors, “We do not know how much virus is actually needed to infect a human being with high probability, nor how easily the virus is transferred from the cardboard to one’s hand when touching a package”
According to Dr. Auwaerter, “It’s thought that this virus can survive on surfaces such as hands, hard surfaces, and fabrics. Preliminary data indicates up to 72 hours on hard surfaces like steel and plastic, and up to 12 hours on fabric.”
COVID-19 will likely “burn off” in the summer
Due to COVID-19’s sensitivity to UV light and heat (just like the normal influenza virus), it is very likely that it will “burn off” as humidity increases and temperatures rise.
Released on March 10th, one study mapped COVID-19 virality capability by high temperature and high humidity. It found that both significantly reduced the ability of the virus to spread from person-to-person. From the study,
“This result is consistent with the fact that the high temperature and high humidity significantly reduce the transmission of influenza. It indicates that the arrival of summer and rainy season in the northern hemisphere can effectively reduce the transmission of the COVID-19.”
The University of Maryland mapped severe COVID-19 outbreaks with local weather patterns around the world, from the US to China. They found that the virus thrives in a certain temperature and humidity channel. “The researchers found that all cities experiencing significant outbreaks of COVID-19 have very similar winter climates with an average temperature of 41 to 52 degrees Fahrenheit, an average humidity level of 47% to 79% with a narrow east-west distribution along the same 30–50 N” latitude”, said the University of Maryland.
“Based on what we have documented so far, it appears that the virus has a harder time spreading between people in warmer, tropical climates,” said study leader Mohammad Sajadi, MD, Associate Professor of Medicine in the UMSOM, physician-scientist at the Institute of Human Virology and a member of GVN.
In the image below, the zone at risk for a significant community spread in the near-term includes land areas within the green bands.